Diabetes - type 1
Highlights
Type 1 Diabetes
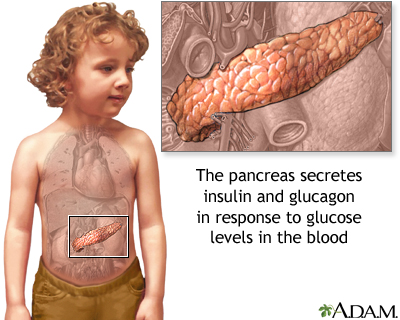
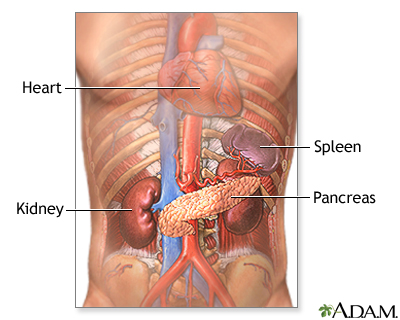
In type 1 diabetes, the pancreas does not produce insulin. Insulin is a hormone that is involved in regulating how the body converts sugar (glucose) into energy. People with type 1 diabetes need to take daily insulin shots and carefully monitor their blood glucose levels.
Type 1 diabetes is much less common than type 2 diabetes. It accounts for 5 - 10% of all diabetes cases. Type 1 diabetes can occur at any age, but it usually first develops in childhood or adolescence.
Symptoms of Diabetes
Symptoms of both type 1 and type 2 diabetes include:
- Frequent urination
- Excessive thirst
- Extreme hunger
- Sudden weight loss
- Extreme fatigue
- Irritability
- Blurred vision
In general, the symptoms of type 1 diabetes come on more abruptly and are more severe than those of type 2 diabetes.
Warning Signs of Hypoglycemia
Hypoglycemia (low blood sugar) occurs when blood sugar (glucose) levels fall below normal. All patients with diabetes should be aware of these symptoms of hypoglycemia:
- Sweating
- Trembling
- Hunger
- Rapid heartbeat
- Confusion
It is important to quickly treat hypoglycemia and raise blood sugar levels by eating sugar, sucking on hard candy, or drinking fruit juice. Patients who are at risk for hypoglycemia should carry some sugar product, or an emergency glucagon injection kit, in case an attack occurs. In rare and worst cases, hypoglycemia can lead to coma and death. Regular blood sugar monitoring throughout the day can help you avoid hypoglycemia. Patients are also encouraged to wear a medical alert ID bracelet or necklace that states they have diabetes and that they take insulin.
Patients with Type 1 Diabetes Living Longer and Healthier Lives
Rates of serious complications among people with type 1 diabetes have decreased over the past several decades. Better control of blood sugar, new treatment strategies, and improved management of co-existing conditions such as high blood pressure appear to have contributed to this positive change.
Introduction
The two major forms of diabetes are type 1, previously called insulin-dependent diabetes mellitus (IDDM) or juvenile-onset diabetes, and type 2, previously called non-insulin-dependent diabetes mellitus (NIDDM) or maturity-onset diabetes.
Insulin
Both type 1 and type 2 diabetes share one central feature: elevated blood sugar (glucose) levels due to absolute or relative insufficiencies of insulin, a hormone produced by the pancreas. Insulin is a key regulator of the body's metabolism. It works in the following way:
- During and immediately after a meal, digestion breaks carbohydrates down into sugar molecules (of which glucose is one) and proteins into amino acids.
- Right after the meal, glucose and amino acids are absorbed directly into the bloodstream, and blood glucose levels rise sharply. (Glucose levels after a meal are called postprandial levels.)
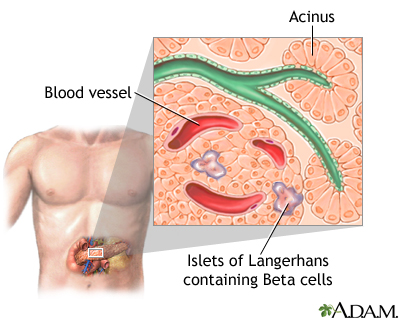
- The rise in blood glucose levels signals important cells in the pancreas, called beta cells, to secrete insulin, which pours into the bloodstream. Within 20 minutes after a meal insulin rises to its peak level.
- Insulin enables glucose to enter cells in the body, particularly muscle and liver cells. Here, insulin and other hormones direct whether glucose will be burned for energy or stored for future use.
- When insulin levels are high, the liver stops producing glucose and stores it in other forms until the body needs it again.
- As blood glucose levels reach their peak, the pancreas reduces the production of insulin.
- About 2 - 4 hours after a meal both blood glucose and insulin are at low levels, with insulin being slightly higher. The blood glucose levels are then referred to as fasting blood glucose concentrations.
Type 1 Diabetes
In type 1 diabetes, the pancreas does not produce insulin. Onset is usually in childhood or adolescence. Type 1 diabetes is considered an autoimmune disorder that involves:
- Beta cells in the pancreas that produce insulin are gradually destroyed. Eventually insulin deficiency is absolute.
- Without insulin to move glucose into cells, blood glucose levels become excessively high, a condition known as hyperglycemia.
- Because the body cannot utilize the sugar, it spills over into the urine and is lost.
- Weakness, weight loss, frequent urination, and excessive hunger and thirst are among the initial symptoms.
- Patients with type 1 diabetes need to take daily insulin for survival.
Type 2 Diabetes
Type 2 diabetes is the most common form of diabetes, accounting for 90 - 95% of cases. In type 2 diabetes, the body does not respond properly to insulin, a condition known as insulin resistance. Over time, the pancreas may become unable to produce insulin in adequate amounts.
Gestational Diabetes
Gestational diabetes is a form of type 2 diabetes, usually temporary, that appears during pregnancy. It usually develops during the third trimester of pregnancy. After delivery, blood sugar (glucose) levels generally return to normal, although some women go on to develop type 2 diabetes.
Gestational diabetes is not the same as the situation for women who have type 1 or type 2 diabetes before their pregnancies.
Causes
Autoimmune Response
Type 1 diabetes is considered a progressive autoimmune disease, in which the beta cells that produce insulin are slowly destroyed by the body's own immune system. It is unknown what first starts this process. Evidence suggests that both a genetic predisposition and environmental factors, such as a viral infection, are involved.
Genetic Factors
Researchers have found at least 18 genetic locations, labeled IDDM1 - IDDM18, which are related to type 1 diabetes. The IDDM1 region contains the HLA genes that encode proteins called major histocompatibility complex. The genes in this region affect the immune response. Other chromosomes and genes continue to be identified.
Most people who develop type 1 diabetes do not have a family history of the disease. The odds of inheriting the disease are only 10% if a first-degree relative has diabetes and, even in identical twins, one twin has only a 33% chance of having type 1 diabetes if the other twin has it. Children are more likely to inherit the disease from a father with type 1 diabetes than from a mother with the disorder.
Genetic factors cannot fully explain the development of diabetes. For the past several decades, the number of new cases of type 1 diabetes has been increasing each year worldwide.
Viruses
Some research suggests that viral infections may trigger the disease in genetically susceptible individuals.
Among the viruses under scrutiny are enteric viruses, which attack the intestinal tract. Coxsackie viruses are a family of enteric viruses of particular interest. Epidemics of Coxsackie virus, as well as mumps and congenital rubella, have been associated with type 1 diabetes.
Risk Factors
Type 1 diabetes is much less common than type 2 diabetes, consisting of only 5 - 10% of all cases of diabetes. Nevertheless, like type 2 diabetes, new cases of type 1 diabetes have been rising over the past few decades. While type 2 diabetes has been increasing among African-American and Hispanic adolescents, the highest rates of type 1 diabetes are found among Caucasian youth.
Type 1 diabetes can occur at any age but usually appears between infancy and the late 30s, most typically in childhood or adolescence. Males and females are equally at risk. Studies report the following may be risk factors for developing type 1 diabetes:
- Being ill in early infancy
- Having a parent with type 1 diabetes (the risk is greater if a father has the condition)
- Having an older mother
- Having a mother who had preeclampsia during pregnancy
- Having other autoimmune disorders such as Grave's disease, Hashimoto's thyroiditis (a form of hypothyroidism), Addison's disease, multiple sclerosis (MS), or pernicious anemia
Symptoms
The process that destroys the insulin-producing beta cells can be long and invisible. At the point when insulin production bottoms out, however, type 1 diabetes usually appears suddenly and progresses quickly. Warning signs of type 1 diabetes include:
- Frequent urination (in children, a recurrence of bed-wetting after toilet training has been completed)
- Unusual thirst, especially for sweet, cold drinks
- Extreme hunger
- Sudden, sometimes dramatic, weight loss
- Weakness
- Extreme fatigue
- Blurred vision or other changes in eyesight
- Irritability
- Nausea and vomiting
Children with type 1 diabetes may also be restless, apathetic, and have trouble functioning at school. In severe cases, diabetic coma may be the first sign of type 1 diabetes.
Complications
Type 1 diabetes increases the risk for many serious health complications. However, during the past several decades, the rate of serious complications among people with diabetes has been decreasing, and more patients are living longer and healthier lives. There are two important approaches to preventing complications from type 1 diabetes:
- Good control of blood glucose and keeping glycosylated hemoglobin (A1C) levels below or around 7%. This approach can help prevent complications due to vascular (blood vessel) abnormalities and nerve damage (neuropathy) that can cause major damage to organs, including the eyes, kidneys, and heart.
- Managing risk factors for heart disease. Blood glucose control helps the heart, but it is also very important that people with diabetes control blood pressure, cholesterol levels, and other factors associated with heart disease.
Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) is a life-threatening complication caused by a complete (or almost complete) lack of insulin. In DKA, the body produces abnormally high levels of blood acids called ketones. Ketones are byproducts of fat breakdown that build up in the blood and appear in the urine. They are produced when the body burns fat instead of glucose for energy. The buildup of ketones in the body is called ketoacidosis. Extreme stages of diabetic ketoacidosis can lead to coma and death.
For some people, DKA may be the first sign that someone has diabetes. In type 1 diabetes, it usually occurs when a patient is not compliant with insulin therapy or intentionally reduces insulin doses in order to lose weight. It can also be triggered by a severe illness or infection.
Symptoms and complications include:
- Thirst and dry mouth
- Frequent urination
- Fatigue
- Dry warm skin
- Nausea and vomiting and stomach pain
- Deep and rapid breathing sometimes with frequent sighing
- Fruity breath odor
- Confusion and decreased consciousness
- Cerebral edema, or brain swelling, is a rare but very dangerous complication that can result in coma, brain damage, or death.
- Other serious complications from DKA include aspiration pneumonia and adult respiratory distress syndrome.
Life-saving treatment uses rapid replacement of fluids with a salt (saline) solution followed by low-dose insulin and potassium replacement.

Hyperglycemic Hyperosmolar Nonketonic Syndrome (HHNS)
Hyperglycemic hyperosmolar nonketonic syndrome (HHNS) is a serious complication of diabetes that involves a cycle of increasing blood sugar levels and dehydration, without ketones. HHNS usually occurs with type 2 diabetes, but it can also occur with type 1 diabetes. It is often triggered by a serious infection or another severe illness, or by medications that lower glucose tolerance or increase fluid loss (especially in people who are not drinking enough fluids).
Symptoms of HHNS include high blood sugar levels, dry mouth, extreme thirst, dry skin, and high fever. HHNS can lead to loss of consciousness, seizures, coma, and death.
Hypoglycemia
Tight blood sugar (glucose) control increases the risk of low blood sugar (hypoglycemia). Hypoglycemia occurs if blood glucose levels fall below normal. It is generally defined as a blood sugar below 70 mg/dL, although this level may not necessarily cause symptoms in all patients. Insufficient intake of food and excess exercise or alcohol intake may cause hypoglycemia. Usually the condition is manageable, but, occasionally, it can be severe or even life threatening, particularly if the patient fails to recognize the symptoms, especially while continuing to take insulin or other hypoglycemic drugs. Beta-blocking medications, which are often prescribed for high blood pressure and heart disease, can mask symptoms of hypoglycemia.
Risk Factors for Severe Hypoglycemia. Specific risk factors for severe hypoglycemia include:
- Patients attempting tight control of blood glucose and A1C levels
- Long-term diabetes
- Patients who do not comply with treatment
- Infections such as gastroenteritis or respiratory illnesses
Hypoglycemia unawareness. Hypoglycemia unawareness is a condition in which people become accustomed to hypoglycemic symptoms. They may no longer notice the signs of hypoglycemia until they become more severe. It affects about 25% of patients who use insulin, nearly always people with type 1 diabetes. In such cases, hypoglycemia appears suddenly, without warning, and can escalate to a severe level. Even a single recent episode of hypoglycemia may make it more difficult to detect the next episode. With vigilant monitoring and by rigorously avoiding low blood glucose levels, patients can often regain the ability to sense the symptoms. However, even very careful testing may fail to detect a problem, particularly one that occurs during sleep.
Symptoms. Mild symptoms usually occur at moderately low and easily correctable levels of blood glucose. They include:
- Sweating
- Trembling
- Hunger
- Rapid heartbeat
Severely low blood glucose levels can cause neurologic symptoms, such as:
- Confusion
- Weakness
- Disorientation
- Combativeness
- In rare and worst cases, coma, seizure, and death
[For information on preventing hypoglycemia or managing an attack, see Home Management section of this report.]
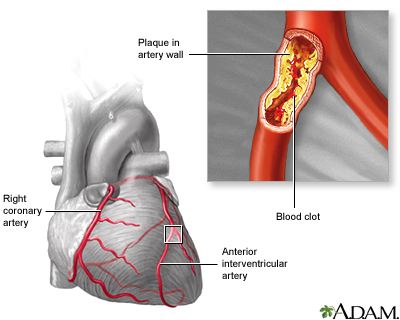
Heart Disease and Stroke
Patients with type 1 diabetes are 10 times more at risk for heart disease than healthy patients. Heart attacks account for 60% of deaths in patients with diabetes, while strokes account for 25% of such deaths. Diabetes affects the heart in many ways:
- Both type 1 and 2 diabetes accelerate the progression of atherosclerosis (hardening of the arteries). Diabetes is often associated with low HDL ("good" cholesterol) and high triglycerides. This can lead to coronary artery disease, heart attack, or stroke.
- In type 1 diabetes, high blood pressure (hypertension) usually develops if the kidneys become damaged. High blood pressure is another major cause of heart attack, stroke, and heart failure. Children with diabetes are also at risk for hypertension.
- Impaired nerve function (neuropathy) associated with diabetes also causes heart abnormalities.
Kidney Damage (Nephropathy)
Kidney disease (nephropathy) is a very serious complication of diabetes. With this condition, the tiny filters in the kidney (called glomeruli) become damaged and leak protein into the urine. Over time this can lead to kidney failure. Urine tests showing microalbuminuria (small amounts of protein in the urine) are important markers for kidney damage.
Diabetic nephropathy is the leading cause of end-stage renal disease (ESRD). Patients with ESRD have 13 times the risk of death compared to other patients with type 1 diabetes. If the kidneys fail, dialysis or transplantation is required. Symptoms of kidney failure may include swelling in the feet and ankles, itching, fatigue, and pale skin color. The outlook of end-stage renal disease has greatly improved during the last four decades for patients with type 1 diabetes, and fewer people with type 1 diabetes are developing ESRD.
Neuropathy
Diabetes reduces or distorts nerve function, causing a condition called neuropathy. Neuropathy refers to a group of disorders that affect nerves. The two main types of neuropathy are:
- Peripheral (affects nerves in the toes, feet, legs, hand, and arms)
- Autonomic (affects nerves that help regulate digestive, bowel, bladder, heart, and sexual function)
Peripheral neuropathy particularly affects sensation. It is a common complication for nearly half of people who have lived with type 1 or type 2 diabetes for more than 25 years. The most serious consequences of neuropathy occur in the legs and feet and pose a risk for ulcers and, in unusually severe cases, amputation. Peripheral neuropathy usually starts in the fingers and toes and moves up to the arms and legs (called a stocking-glove distribution). Symptoms include:
- Tingling
- Weakness
- Burning sensations
- Loss of the sense of warm or cold
- Numbness (if the nerves are severely damaged, the patient may be unaware that a blister or minor wound has become infected)
- Deep pain
Autonomic neuropathy can cause:
- Digestive problems (such as constipation, diarrhea, nausea, and vomiting)
- Bladder infections and incontinence
- Erectile dysfunction
- Heart problems. Neuropathy may mask angina, the warning chest pain for heart disease and heart attack. Patients with diabetes should be aware of other warning signs of a heart attack, including sudden fatigue, sweating, shortness of breath, nausea, and vomiting.
- Rapid heart rates
- Lightheadedness when standing up (orthostatic hypotension)
Diabetic gastroparesis is a type of neuropathy that affects the digestive track. It is triggered by high blood sugar, which over time can damage the vagus nerve. The result of this damage is that the digestive system takes too long at time to move and empty food. Undigested food and the delay in stomach emptying can cause blood glucose levels to rise, and make diabetes more difficult to control. Symptoms of gastroparesis include heartburn, nausea, abdominal bloating, feeling full after eating only a small amount of food, and vomiting of undigested food several hours after a meal.
Blood sugar control is an essential component in the treatment for neuropathy. Studies show that tight control of blood glucose levels delays the onset and slows progression of neuropathy. Heart disease risk factors may increase the likelihood of developing neuropathy. Lowering triglycerides, losing weight, reducing blood pressure, and quitting smoking may help prevent the onset of neuropathy.
Foot Ulcers and Amputations
About 15% of patients with diabetes have serious foot problems. They are the leading cause of hospitalizations for these patients. The consequences of both poor circulation and peripheral neuropathy make this a common and serious problem for all patients with diabetes. Diabetes is responsible for more than half of all lower limb amputations performed in the U.S. Most amputations start with foot ulcers.
People with diabetes who are overweight, smokers, and have a long history of diabetes tend to be at most risk. People who have the disease for more than 20 years and are insulin-dependent are at the highest risk. Related conditions that put people at risk include peripheral neuropathy, peripheral artery disease, foot deformities, and a history of ulcers.
Foot ulcers usually develop from infections, such as those resulting from blood vessel injury. Numbness from nerve damage, which is common in diabetes, compounds the danger since the patient may not be aware of injuries. About one-third of foot ulcers occur on the big toe.
Charcot Foot. Charcot foot or Charcot joint (medically referred to as neuropathic arthropathy) is a degenerative condition that affects the bones and joints in the feet. It is associated with the nerve damage that occurs with neuropathy. Early changes appear similar to an infection, with the foot becoming swollen, red, and warm. Gradually, the affected foot can become deformed. The bones may crack, splinter, and erode, and the joints may shift, change shape, and become unstable. It typically develops in people who have neuropathy to the extent that they cannot feel sensation in the foot and are not aware of an existing injury. Instead of resting an injured foot or seeking medical help, the patient often continues normal activity, causing further damage.
Retinopathy and Eye Complications
Diabetes accounts for thousands of new cases of blindness annually and is the leading cause of new cases of blindness in adults ages 20 - 74. The most common eye disorder in diabetes is retinopathy. People with diabetes are also at higher risk for developing cataracts and certain types of glaucoma.
Retinopathy is a condition in which the retina becomes damaged. It generally occurs in one or two phases:
- The early and more common type of this disorder is called nonproliferative or background retinopathy. The blood vessels in the retina are abnormally weakened. They rupture and leak, and waxy areas may form. If these processes affect the central portion of the retina, swelling may occur, causing reduced or blurred vision.
- If the capillaries become blocked and blood flow is cut off, soft, "woolly" areas may develop in the retina's nerve layer. These woolly areas may signal the development of proliferative retinopathy. In this more severe condition, new abnormal blood vessels form and grow on the surface of the retina. They may spread into the cavity of the eye or bleed into the back of the eye. Major hemorrhage or retinal detachment can result, causing severe visual loss or blindness. The sensation of seeing flashing lights may indicate retinal detachment.
Infections
Respiratory Infections. People with diabetes face a higher risk for influenza and its complications, including pneumonia. Everyone with diabetes should have annual influenza vaccinations and a vaccination against pneumococcal pneumonia.
Urinary Tract Infections. Women with diabetes face a significantly higher risk for urinary tract infections, which are likely to be more complicated and difficult to treat than in the general population.
Hepatitis. Patients with diabetes are at increased risk for contracting the hepatitis B virus, which is transmitted through blood and other bodily fluids. Exposure to the virus can occur through sharing finger-stick devices or blood glucose monitors. Adults newly diagnosed with type 1 or type 2 diabetes should get hepatitis B vaccinations.
Depression
Diabetes doubles the risk for depression. Depression, in turn, may increase the risk for hyperglycemia and complications of diabetes.
Osteoporosis
Type 1 diabetes is associated with slightly reduced bone density, putting patients at risk for osteoporosis and possibly fractures.
Other Complications
Diabetes increases the risk for other conditions, including:
- Hearing loss
- Periodontal disease
- Carpal tunnel syndrome and other nerve entrapment syndromes
- Nonalcoholic fatty liver disease, also called nonalcoholic steatohepatitis (NASH); a particular danger for people who are obese
Specific Complications in Women
Diabetes can cause specific complications in women. Women with diabetes have an increased risk of recurrent yeast infections. In terms of sexual health, diabetes may cause decreased vaginal lubrication, which can lead to pain or discomfort during intercourse.
Women with diabetes should also be aware that certain types of medication can affect their blood glucose levels. For example, birth control pills can raise blood glucose levels. Long-term use (more than 2 years) of birth control pills may increase the risk of health complications.
Diabetes and Pregnancy. Pregnancy in a patient with existing diabetes can increase the risk for birth defects. Studies indicate that high blood sugar levels (hyperglycemia) can affect the developing fetus during the critical first 6 weeks of organ development. Therefore, it is important that women with pre-existing diabetes (both type 1 and type 2) who are planning on becoming pregnant strive to maintain good glucose control for 3 - 6 months before pregnancy.
It is also important for women to closely monitor their blood sugar levels during pregnancy. For women with type 1 diabetes, pregnancy can affect their insulin dosing needs. Insulin dosing may also need to be adjusted during and following delivery. [For more information, see “Treatment of Diabetes During Pregnancy” in Treatment of Complications section of this report.]
Diabetes and Menopause. The changes in estrogen and other hormonal levels that occur during perimenopause can cause major fluctuations in blood glucose levels. Women with diabetes also face an increased risk of premature menopause, which can lead to higher risk of heart disease.
Specific Problems for Adolescents with Type 1 Diabetes
Lack of Blood Glucose Control. Control of blood glucose levels is generally very poor in adolescents and young adults. Adolescents with diabetes are at higher risk than adults for ketoacidosis resulting from noncompliance. Young people who do not control glucose are also at high risk for permanent damage in small vessels, such as those in the eyes.
Eating Disorders. Up to a third of young women with type 1 diabetes have eating disorders and under-use insulin to lose weight. Anorexia and bulimia pose significant health risks in any young person, but they can be especially dangerous for people with diabetes.
Diagnosis
There are three tests that can diagnose diabetes:
- Fasting plasma glucose (FPG)
- Oral glucose tolerance test (OGTT)
- Hemoglobin A1C (A1C)
Fasting Plasma Glucose Test
The fasting plasma glucose (FPG) test has been the standard test for diagnosing diabetes. It is a simple blood test taken after 8 hours of fasting.
FPG levels indicate:
- Normal. Below 100 mg/dL (or 5.5 mmol/L).
- Pre-Diabetes. (A risk factor for type 2 diabetes): Between 100 - 125 mg/dL (5.5 - 7.0 mmol/L).
- Diabetes.126 mg/dL (7.0 mmol/L) or higher.
The FPG test is not always reliable, so a repeat test is recommended if the initial test suggests the presence of diabetes, or if the tests are normal in people who have symptoms or risk factors for diabetes. Widespread screening of patients to identify those at higher risk for diabetes type 1 is not recommended.
Oral Glucose Tolerance Test
The oral glucose tolerance test (OGTT) is more complex than the FPG and may overdiagnose diabetes in people who do not have it. Some doctors recommend it as a follow-up after FPG, if the latter test results are normal but the patient has symptoms or risk factors of diabetes. The test uses the following procedures:
- It first uses an FPG test.
- A blood test is then taken 2 hours later after drinking a special glucose solution.
OGTT levels indicate:
- Normal. Below 140 mg/dL.
- Pre-Diabetes. Between 140 - 199 mg/dL,
- Diabetes. 200 mg/dL or higher.
Patients who have the FPG and OGTT tests must not eat for at least 8 hours prior to the test.

Hemoglobin A1C Test
This test examines blood levels of glycosylated hemoglobin, also known as hemoglobin A1C (HbA1c). The results are given in percentages and indicate a person’s average blood glucose levels over the past 2 - 3 months. (The FPG and OGTT show a person’s glucose level for only the time of the test.) The A1C test is not affected by recent food intake so patients do not need to fast to prepare for it.
In 2010, the American Diabetes Association advised that the A1C test can be used as another option for diagnosing diabetes.
A1C levels indicate:
- Normal. Below 5.7 percent.
- Pre-Diabetes. Between 5.7 - 6.4 percent.
- Diabetes. 6.5 percent or higher.
A1C tests are also used to help patients with diabetes monitor how well they are keeping their blood glucose levels under control. For patients with diabetes, A1C is measured periodically every 2 - 3 months, or at least twice a year. While finger prick self-testing provides information on blood glucose for that day, the A1C test shows how well blood sugar has been controlled over the past several months.
In general, most adult patients with diabetes should aim for A1C levels below or around 7%. Your doctor may adjust this goal depending on your individual health profile.
Goal A1C levels for children are:
- Between 7.5 - 8.5% for children under age 6 years
- Less than 8% for children age 6 - 12 years
- Less than 7.5% for children age 13 - 19 years
Schedule for A1C Monitoring:
- Every 6 months if diabetes is well controlled
- Every 3 months if not well controlled
The American Diabetes Association recommends that results from the A1C test be used as to calculate estimated Average Glucose (eAG). EAG is a relatively new term that patients may see on lab results from their A1C tests. It converts the A1C percentages into the same mg/dL units that patients are familiar with from their daily home blood glucose tests. For example, an A1C of 7% is equal to an eAG of 154 mg/dL. The eAG terminology can help patients better interpret the results of their A1C tests, and make it easier to correlate A1C with results from home blood glucose monitoring.
Autoantibody Tests
Type 1 diabetes is characterized by the presence of a variety of antibodies that attack the islet cells. These antibodies are referred to as autoantibodies because they attack the body's own cells -- not a foreign invader. Blood tests for these autoantibodies can help differentiate between type 1 and type 2 diabetes.
Screening Tests for Complications
Screening Tests for Heart Disease. All patients with diabetes should be tested for high blood pressure (hypertension) and unhealthy cholesterol and lipid levels and given an electrocardiogram. Other tests may be needed in patients with signs of heart disease.
Screening Tests for Kidney Damage. The earliest manifestation of kidney disease is microalbuminuria, in which tiny amounts of a protein called albumin are found in the urine. Microalbuminuria is also a marker for other complications involving blood vessel abnormalities, including heart attack and stroke.
People with diabetes should have an annual microalbuminuria urine test. Patients should also have their blood creatinine tested at least once a year. Creatinine is a waste product that is removed from the blood by the kidneys. High levels of creatinine may indicate kidney damage. A doctor uses the results from a creatinine blood test to calculate the glomerular filtration rate (GFR). The GFR is an indicator of kidney function; it estimates how well the kidneys are cleaning the blood.
Screening for Retinopathy. The American Diabetes Association recommends that patients with type 1 diabetes have an annual comprehensive eye exam, with dilation, to check for signs of retina disease (retinopathy). Patients at low risk may need exams only every 2 - 3 years. In addition to a comprehensive eye exam, fundus photography may be used as a screening tool. Fundus photography uses a special type of camera to take images of the back of the eye.
Screening for Neuropathy. All patients should be screened for nerve damage (neuropathy), including a comprehensive foot exam. Patients who lose sensation in their feet should have a foot exam every 3 - 6 months to check for ulcers or infections.
Screening for Thyroid Abnormalities. Thyroid function tests should be performed.
Lifestyle Changes
Good nutrition and regular exercise can help prevent or manage medical complications of diabetes (such as heart disease and stroke), and help patients live longer and healthier lives.
Diet
There is no single diabetes diet. Patients should meet with a professional dietitian to plan an individualized diet within the general guidelines that takes into consideration their own health needs.
Healthy eating habits, along with good control of blood glucose, are the basic goals, and several good dietary methods are available to meet them. General dietary guidelines for diabetes recommend:
- Carbohydrates should provide 45 - 65% of total daily calories. The type and amount of carbohydrate are both important. Best choices are vegetables, fruits, beans, and whole grains. These foods are also high in fiber. Patients with diabetes should monitor their carbohydrate intake either through carbohydrate counting or meal planning exchange lists.
- Fats should provide 25 - 35% of daily calories. The best types of fats are monounsaturated (olive, peanut, and canola oils; avocados; and nuts) and omega-3 polyunsaturated (fish, flaxseed oil, and walnuts). Limit saturated fat (red meat, butter) to less than 7% of daily calories. Choose nonfat or low-fat dairy instead of whole milk products. Limit trans-fats (hydrogenated fat found in snack foods, fried foods, and commercially baked goods) to less than 1% of total calories.
- Protein should provide 12 - 20% of daily calories, although this may vary depending on a patient’s individual health requirements. Patients with kidney disease should limit protein intake to less than 10% of calories. Fish, soy, and poultry are better protein choices than red meat.
- Sodium (salt) intake should be limited to 1,500 mg/day or less. Reducing sodium can help lower blood pressure and decrease the risk of heart disease.
Healthy Weight Control
Weight gain is a potential side effect of intense diabetic control with insulin. Being overweight can increase the risk for health problems. On the other hand, studies suggest that more than one-third of women with diabetes omit or underuse insulin in order to lose weight. Eating disorders are especially dangerous in patients with diabetes and can increase the risk for diabetic ketoacidosis. Ketoacidosis is a significant complication of insulin depletion and can be life threatening.
Exercise
Aerobic exercise has significant and particular benefits for people with type 1 diabetes. It increases sensitivity to insulin, lowers blood pressure, improves cholesterol levels, and decreases body fat. Because glucose levels swing dramatically during workouts, people with type 1 diabetes need to take certain precautions:
- Monitor glucose levels carefully before, during, and after workouts.
- Avoid exercise if glucose levels are above 300 mg/dL or under 100 mg/dL.
- To avoid hypoglycemia, patients should inject insulin in sites away from the muscles they use the most during exercise.
- Before exercising, avoid alcohol and if possible certain drugs, including beta blockers, which make it difficult to recognize symptoms of hypoglycemia.
- Insulin-dependent athletes may need to decrease insulin doses or take in more carbohydrates, especially in the form of pre-exercise snacks. Skim milk is particularly helpful. They should also drink plenty of fluids.
- Good, protective footwear is essential to help avoid injuries and wounds to the feet.
Avoid resistance or high impact exercises. They can strain weakened blood vessels in the eyes of patients with retinopathy. High-impact exercise may also injure blood vessels in the feet. Because patients with diabetes may have silent heart disease, they should always check with their doctors before undertaking vigorous exercise.
Warning on Dietary Supplements
Various fraudulent products are often sold on the Internet as “cures” or treatments for diabetes. These dietary supplements have not been studied or approved. The US Food and Drug Administration (FDA) and Federal Trade Commission (FTC) warn patients with diabetes not to be duped by bogus and unproven remedies.
Treatment
Insulin is essential for control of blood glucose levels in type 1 diabetes. Good blood glucose control is the best way to prevent major complications in type 1 diabetes, including those that affect the kidneys, eyes, nerve pathways, and blood vessels. Intensive insulin treatment in early diabetes may even help preserve any residual insulin secretion for at least 2 years.
There are, however, some significant problems with intensive insulin therapy:
- There is a greater risk for low blood sugar (hypoglycemia).
- Many patients experience significant weight gain from insulin administration, which may have adverse effects on blood pressure and cholesterol levels. It is important to manage heart disease risk factors that might develop as a result of insulin treatment.
A diet plan that compensates for insulin administration and supplies healthy foods is extremely important. Pancreas transplantation may eventually be considered for patients who cannot control glucose levels without frequent episodes of severe hypoglycemia.
Regimens for Intensive Insulin Treatment
The goal of intensive insulin therapy is to keep blood glucose levels as close to normal as possible.
Glucose Goals for Patients with Diabetes | ||
Normal | Goal | |
Blood glucose levels before meals | Less than 100 mg/dL | 70 - 130 mg/dL for adults 100 - 180 mg/dL for children under age 6 90 - 180 mg/dL for children 6 - 12 years old 90 - 130 mg/dL for children 13 - 19 years old |
Bedtime blood glucose levels | Less than 120 mg/dL | Less than 180 mg/dL for adults 110 - 200 mg/dL for children under age 6 100 - 186 mg/dL for children 6 - 12 years old 90 - 150 mg/dL for children 13 - 19 years old |
Glycosylated hemoglobin (A1C) levels | Less than 5.7% | Less than or around 7% |
Major source: Standards of Medical Care In Diabetes -- 2012, American Diabetes Association. | ||
Standard insulin therapy usually consists of one or two daily insulin injections, one daily blood sugar test, and visits to the health care team every 3 months. For strictly controlling blood glucose, however, intensive management is required. The regimen is complicated although newer insulin forms may make it easier.
There are two components to insulin administration:
- Basal insulin administration. The basal component of the treatment attempts to provide a steady amount of background insulin throughout the day. Basal insulin levels maintain regular blood glucose needs. Insulin glargine offers the most consistent insulin activity level, but other intermediate and long-acting forms may be beneficial when administered twice a day. Short-acting insulin delivered continuously using a pump is proving to a very good way to provide basal rates of insulin.
- Mealtime insulin administration. Meals require a boost (a bolus) of insulin to regulate the sudden rise in glucose levels after a meal.
In achieving insulin control the patient must also take other steps:
- Perform four or more blood glucose tests during the day.
- Coordinate insulin administration with calorie intake. In general, eat three meals each day at regular intervals. Snacks are often necessary.
- Insulin requirements vary depending on many non-nutritional situations during the day, including exercise and sleep. Exercise increases the risk for low blood sugar. Some patients experience a sudden rise in blood glucose levels in the morning -- the so-called "dawn phenomenon."
- It is important to maintain a good diet plan and visit your health care team (doctor, nurse, dietitian) once a month.
Because of the higher risk for hypoglycemia in children, doctors recommend that intensive insulin treatment be used very cautiously in children under 13 and not at all in very young children.
Types of Insulin
Insulin cannot be taken orally because the body's digestive juices destroy it. Injections of insulin under the skin ensure that it is absorbed slowly by the body for a long-lasting effect. The timing and frequency of insulin injections depend upon a number of factors:
- The duration of insulin action. Insulin is available in several forms, including: standard, intermediate, long-acting, and rapid-acting.
- Amount and type of food eaten. Ingestion of food makes the blood glucose level rise. Alcohol lowers levels.
- A person's level of physical activity. Exercise lowers glucose levels.
Fast-Acting Insulin. Insulin lispro (Humalog) and insulin aspart (Novo Rapid, Novolog) lower blood sugar very quickly, usually within 5 minutes after injection. Insulin peaks in about 4 hours and continues to work for about 4 more hours. This rapid action reduces the risk for hypoglycemic events after eating (postprandial hypoglycemia). Optimal timing for administering this insulin is about 15 minutes before a meal, but it can also be taken immediately after a meal (but within 30 minutes). Fast-acting insulins may be especially useful for meals with high carbohydrates.
Regular Insulin. Regular insulin begins to act 30 minutes after injection, reaches its peak at 2 - 4 hours, and lasts about 6 hours. Regular insulin may be administered before a meal and may be better for high-fat meals.
Intermediate Insulin. NPH (Neutral Protamine Hagedorn) insulin has been the standard intermediate form. It works within 2 - 4 hours, peaks 4 - 12 hours later, and lasts up to 18 hours. Lente (insulin zinc) is another intermediate insulin that peaks 4 - 12 hours and lasts up to 18 hours.
Long-Acting (Ultralente) Insulin. Long-acting insulins, such as insulin glargine (Lantus), are released slowly. Long-acting insulin peaks at 10 hours and lasts up to 20 hours. Researchers are studying new types of long-acting insulins including one called degludec that requires injections only three times a week.
Combinations. Regimens generally include combinations of short and longer-acting insulins to help match the natural cycle. For example, one approach in patients who are intensively controlling their glucose levels uses 3 injections of insulin, which includes a mixture of regular insulin and NPH at dinner. Another approach uses 4 injections, including a separate short-acting form at dinner and NPH at bedtime, which may pose a lower risk for nighttime hypoglycemia than the 3-injection regimen.
Insulin Pens. Insulin pens, which contain cartridges of insulin, have been available for some time. Until recently, they were fairly complicated and difficult to use. Newer, prefilled pens (Humulin Pen, Humalog) are disposable and allow the patient to dial in the correct amount.
Insulin Pumps
An insulin pump can improve blood glucose control and quality of life with fewer hypoglycemic episodes than multiple injections. The pumps correct for the “dawn phenomenon” (sudden rise of blood glucose in the morning) and allow quick reductions for specific situations, such as exercise. Many different brands are available.
The typical pump is about the size of a beeper and has a digital display. Some are worn externally and are programmed to deliver insulin through a catheter in the skin or the abdomen. They generally use rapid-acting insulin, the most predictable type. They work by administering a small amount of insulin continuously (the basal rate) and a higher dose (a bolus dose) when food is eaten.
Although learning to use the pump can be complicated at first, most patients find over time that the devices are fairly easy to use. Adults, adolescents, and school children use insulin pumps and even very young children (ages 2 - 7 years) may be able to successfully use them.
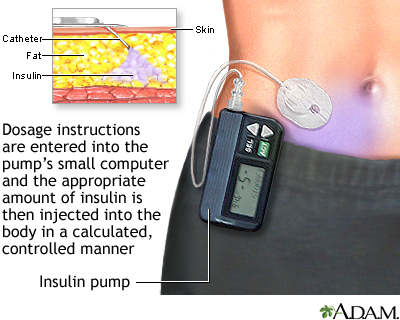
To achieve good blood sugar control, patients and parents of children must undergo some training. The patient and doctor must determine the amount of insulin used -- it is not automatically calculated. This requires an initial learning period, including understanding insulin needs over the course of the day and in different situations and knowledge of carbohydrate counting. Frequent blood testing is very important, particularly during the training period.
Insulin pumps are more expensive than insulin shots and occasionally have some complications, such as blockage in the device or skin irritation at the infusion site. In spite of early reports of a higher risk for ketoacidosis with pumps, more recent studies have found no higher risk.
Supplementary Drugs for Hyperglycemia
Pramlintide (Symlin) is an injectable drug that is used to help control postprandial hyperglycemia, the sudden increase in blood sugar after a meal. Pramlintide is injected before meals and can help lower blood sugar levels in the 3 hours after meals. Pramlintide is used in addition to insulin for patients who take insulin regularly but still need better blood sugar control. Pramlintide and insulin are the only two drugs approved for treatment of type 1 diabetes.
Pramlintide is a synthetic form of amylin, a hormone that is related to insulin. Side effects may include nausea, vomiting, abdominal pain, headache, fatigue, and dizziness. Patients with type 1 diabetes have an increased risk of severe low blood sugar (hypoglycemia) that may occur within 3 hours following a pramlintide injection. This drug should not be used if patients have trouble knowing when their blood sugar is low or have slow stomach emptying (gastroparesis).
Treatment of Complications
High Blood Pressure and Heart Disease
All patients with diabetes and high blood pressure should adopt lifestyle changes. These include weight reduction (when needed), following the Dietary Approaches to Stop Hypertension (DASH) diet, smoking cessation, limiting alcohol intake, and limiting salt intake to no more than 1,500 mg of sodium per day.
High Blood Pressure Control. Patients should aim for blood pressure levels of less than 130/80 mm Hg (systolic/diastolic).
Patients with diabetes and high blood pressure need an individualized approach to drug treatment, based on their particular health profile. Dozens of anti-hypertensive drugs are available. The most beneficial fall into the following categories
- Diuretics rid the body of extra sodium (salt) and water. There are three main types of diuretics: Potassium-sparing, thiazide, and loop.
- Angiotensin-converting enzyme (ACE) inhibitors reduce the production of angiotensin, a chemical that causes arteries to narrow.
- Angiotensin-receptor blockers (ARBs) block angiotensin.
- Beta blockers block the effects of adrenaline and ease the heart’s pumping action.
- Calcium-channel blockers (CCBs) decrease the contractions of the heart and widen blood vessels. Like ACE inhibitors and ARBs, certain calcium channel blockers (diltiazem and verapamil) can reduce urine protein loss caused by diabetic kidneys.
Nearly all patients who have diabetes and high blood pressure should take an ACE inhibitor (or ARB) as part of their regimen for treating their hypertension. These drugs help prevent kidney damage.
Improving Cholesterol and Lipid Levels. Abnormal cholesterol and lipid levels are common in diabetes. High LDL (“bad”) cholesterol should always be lowered, but people with diabetes also often have additional harmful imbalances, including low HDL (“good”) cholesterol and high triglycerides.
Adult patients should aim for LDL levels below 100 mg/dL, HDL levels over 50 mg/dL, and triglyceride levels below 150 mg/dL. Patients with diabetes and existing heart disease should strive for even lower LDL levels; the American Diabetes Association recommends LDL levels below 70 mg/dL for these patients.
Children should be treated for LDL cholesterol above 160 mg/dL, or above 130 mg/dL if they have other cardiovascular risk factors.
For medications, statins are the best cholesterol-lowering drugs. They include atorvastatin (Lipitor, generic), lovastatin (Mevacor, Altoprev, Advicor, generics), pravastatin (Pravachol, generic), simvastatin (Zocor, Simcor, Vytorin, and generics), fluvastatin (Lescol), rosuvastatin (Crestor), and pitavastatin (Livalo). These drugs are very effective for lowering LDL cholesterol levels. However, they may increase blood glucose levels in some patients, especially when taken in high doses. Still, statin drugs are considered generally safe and the best first choice for managing high cholesterol.
The primary safety concern with statins has involved myopathy, an uncommon condition that can cause muscle damage and, in some cases, muscle and joint pain. A specific myopathy called rhabdomyolysis can lead to kidney failure. People with diabetes and risk factors for myopathy should be monitored for muscle symptoms.
Although lowering LDL cholesterol is beneficial, statins are not as effective as other medications -- such as niacin and fibrates -- in addressing HDL and triglyceride imbalances. Combining a statin with one of these drugs may be helpful for people with diabetes who have heart disease, low HDL, and near-normal LDL levels. Although combinations of statins and fibrates or niacin increase the risk of myopathy, both combinations are considered safe if used with extra care.
Fibrates such as gemfibrozil (Lopid, generic), fenofibrate (Tricor, generic), and fenofibric acid (Trilipix) are usually the second choice after statins although it is unclear if they have much benefit in reducing the risk for heart attack and stroke in people with diabetes. Niacin has the most favorable effect on raising HDL and lowering triglycerides of all the cholesterol drugs. However, some patients who take high-dose niacin can experience increased blood glucose levels. Moderate doses of niacin can control lipids without causing serious blood glucose problems.
Aspirin for Heart Disease Prevention. For patients with diabetes who have additional heart disease risk factors, taking a daily aspirin can reduce the risk for blood clotting and may help protect against heart attacks. (There is not enough evidence to indicate that aspirin prevention is helpful for patients at lower risk.) The recommended dose is 75 - 162 mg/day. Aspirin as primary prevention is recommended for men who are older than age 50 or women who are older than age 60 who have at least one additional heart risk factor. These risk factor include a family history of heart disease, high blood pressure, smoking, unhealthy cholesterol levels, or excessive urine levels of the protein albumin (albuminuria). Talk to your doctor, particularly if you are at risk for aspirin side effects such as gastrointestinal bleeding and ulcers.
Treatment of Retinopathy
Patients with severe diabetic retinopathy or macular edema (swelling of the retina) should see an eye specialist who is experienced in the management and treatment of diabetic retinopathy. Once damage to the eye develops, laser or photocoagulation eye surgery may be needed. Laser surgery can help reduce vision loss in high-risk patients.
Treatment of Foot Ulcers
About a third of foot ulcers will heal within 20 weeks with good wound care treatments. Some treatments are as follows:
- Antibiotics are generally given. In some cases, hospitalization and intravenous antibiotics for up to 28 days may be needed for severe foot ulcers.
- In virtually all cases, wound care requires debridement, which is the removal of injured tissue until only healthy tissue remains. Debridement may be accomplished using chemical (enzymes), surgical, or mechanical (irrigation) means.
- Hydrogels (such as Nu-Gel) may help soothe and heal ulcers.
- Felted foam may be helpful in healing ulcers on the sole of the foot. Felted foam uses a multi-layered foam pad over the bottom of the foot with an opening over the ulcer.
Other Treatments for Foot Ulcers. Doctors are also using or investigating other treatments to heal ulcers. These include:
- Administering hyperbaric oxygen (oxygen given at high pressure) is showing promise in promoting healing. It is generally reserved for patients with severe, full thickness diabetic foot ulcers that have not responded to other treatments, particularly when gangrene or an abscess is present.
- Total-contact casting (TCC) uses a cast that is designed to match the exact contour of the foot and distribute weight along the entire length of the foot. It is usually changed weekly. It may be helpful for ulcer healing and for Charcot foot. Although it is very effective in healing ulcers, recurrence is common.
Treatment of Diabetic Neuropathy
The only FDA-approved drugs for treating neuropathy are pregabalin (Lyrica) and duloxetine (Cymbalta). Other drugs and treatments are used on an off-label basis.
The American Academy of Neurology’s (AAN) guidelines for treating painful diabetic neuropathy recommend:
- Anticonvulsants. Pregabalin (Lyrica) is a first-line treatment and has the strongest evidence for efficacy of all neuropathy treatments. Gabapentin (Neurontin, generic) and valproate (Depacon, generic) may also be considered.
- Antidepressants. Duloxetine (Cymbalta) and venlaxafine (Effexor) are recommended, as is amitriptyline (Elavil, generic). Venlafaxine may be given in combination with gabapentin. Duloxetine and venlafaxine are serotonin and norepinephrine reuptake inhibitors. Amitriptyline is a tricyclic antidepressant. Tricyclics may cause heart rhythm problems, so patients at risk need to be monitored carefully.
- Opoids. Opoids are powerful prescription narcotic painkillers. Dextromethorphan, morphine, oxycodone, and tramadol (Ultram, generic) may be considered for severe neuropathy pain. These drugs can cause significant side effects (nausea, constipation, headache) and can be addictive.
- Topical Medications. Capsaicin ointment or a lidocaine skin patch may be effective. These treatments are applied directly to the skin. Capsaicin is the active ingredient in hot chili peppers.
Non-Drug Treatments. Percutaneous electrical nerve stimulation (PENS) may help some patients. PENS uses electrodes attached to precisely placed acupuncture-type needles to deliver electrical current to peripheral sensory nerves. Doctors also recommend lifestyle measures, such as walking and wearing elastic stockings.
Treatments for Other Complications of Neuropathy. Neuropathy also impacts other functions, and treatments are needed to reduce their effects. If diabetes affects the nerves in the autonomic nervous system, then abnormalities of blood pressure control and bowel and bladder function may occur. Erythromycin, domperidone (Motilium), or metoclopramide (Reglan) may be used to relieve delayed stomach emptying caused by neuropathy (diabetic gastroparesis). Patients need to watch their nutrition if the problem is severe.
Erectile dysfunction is also associated with neuropathy. Studies indicate that phosphodiesterase type 5 (PDE-5) drugs, such as sildenafil (Viagra), vardenafil (Levitra), tadalafil (Cialis), and avanafil (Stendra) are safe and effective, at least in the short term, for many patients with diabetes. Typical side effects are minimal but may include headache, flushing, and upper respiratory tract and flu-like symptoms. Patients who take nitrate medications for heart disease cannot use PDE-5 drugs.
Treatment of Kidney Problems
Tight control of blood sugar and blood pressure is essential for preventing the onset of kidney disease and for slowing the progression of the disease.
ACE inhibitors are the best class of blood pressure medications for delaying kidney disease and slowing disease progression in patients with diabetes. Angiotensin-receptor blockers (ARBs) are also very helpful.
- For patients with diabetes who have microalbuminuria, the American Diabetes Association strongly recommends ACE inhibitors or ARBs. Microalbuminuria is an accumulation of protein in the blood, which can signal the onset of kidney disease (nephropathy).
- Nearly all patients who have diabetes and high blood pressure should take an ACE inhibitor (or ARB) as part of their regimen for treating their hypertension
A doctor may recommend a low-protein diet for patients whose kidney disease is progressing despite tight blood sugar and blood pressure control. Protein-restricted diets can help slow disease progression and delay the onset of end-stage renal disease (kidney failure). However, patients with end-stage renal disease who are on dialysis generally need higher amounts of protein.
Anemia.Anemia is a common complication of end-stage kidney disease. Patients on dialysis usually need injections of erythropoiesis-stimulating drugs to increase red blood cell counts and control anemia. However, these drugs -- darbepoetin alfa (Aranesp) and epoetin alfa (Epogen and Procrit) -- can increase the risk of blood clots, stroke, heart attack, and heart failure in patients with end-stage kidney disease when they are given at higher than recommended doses. Peginesatide (Omontys) is a new erythropoiesis-stimulating drug approved specifically for patients with chronic kidney disease who are on dialysis. It is given as a once-a-month injection.
The FDA recommends that patients with end-stage kidney disease who receive erythropoiesis-stimulating drugs should:
- Maintain hemoglobin levels between 10 - 12 g/dL.
- Receive frequent blood tests to monitor hemoglobin levels.
- Contact their doctors if they experience such symptoms as shortness of breath, pain, swelling in the legs, or increases in blood pressure.
Treatment of Diabetes During Pregnancy
Some recommendations for preventing pregnancy complications include:
- Intensive blood sugar control during pregnancy can reduce the risk for health complications for both mothers and babies. Doctors recommend that pregnant women with pre-existing diabetes monitor their blood sugar levels up to 8 times daily. This includes checking your blood glucose before each meal, 1 - 2 hours after a meal, at bedtime, and possibly during the night.
- Insulin needs increase during the pregnancy, especially during the last 3 months. Your doctor may recommend increasing your insulin dosage during this time.
- Consult a registered dietician to help adjust your food plan during pregnancy.
- Low-impact aerobic exercise during pregnancy can lower glucose levels. (All pregnant women, particularly those with diabetes, should check with their doctors before embarking on a rigorous exercise regimen. This is especially important for women with eye, kidney, or high blood pressure or other heart problems.)
- To prevent birth defects that affect the heart and nervous system, women with diabetes should take a higher dose of folic acid from the time of conception up to week 12 of pregnancy. They should also be checked for any heart problems.
- Women with diabetes should have an eye examination during pregnancy and up to a year afterward.
Home Management
Monitoring Glucose (Blood Sugar) Levels
Both low blood sugar (hypoglycemia) and high blood sugar (hyperglycemia) are of concern for patients who take insulin. It is important, therefore, to carefully monitor blood glucose levels. In general, patients with type 1 diabetes need to take readings four or more times a day. Patients should aim for the following measurements:
- Pre-meal glucose levels of 70 - 130 mg/dL
- Post-meal glucose levels of less than 180 mg/dL
Different goals may be required for specific individuals, including pregnant women, very old and very young people, and those with accompanying serious medical conditions.
Finger-Prick Test. A typical blood sugar test includes the following:
- A drop of blood is obtained by pricking the finger.
- The blood is then applied to a chemically treated strip.
- Monitors read and provide results.
Home monitors are less accurate than laboratory monitors and many do not meet the standards of the American Diabetes Association. However, they are usually accurate enough to indicate when blood sugar is too low.
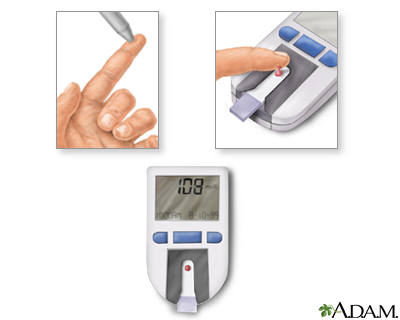
Some simple procedures may improve accuracy:
- Testing the meter once a month.
- Recalibrating it whenever a new packet of strips is used.
- Using fresh strips; outdated strips may not provide accurate results.
- Keeping the meter clean.
- Periodically comparing the meter results with the results from a laboratory.
Continuous Glucose Monitoring Systems
Continuous glucose monitoring systems (CGMs) use a needle-like sensor inserted under the skin of the abdomen to monitor glucose levels every 5 minutes. Depending on the system, CMGs measure glucose levels for 3- 7 days and sound an alarm if glucose levels are too high or low. These devices are used in addition to traditional fingerstick test kits and glucose meters but do not replace them.
Urine Tests
Urine tests are useful for detecting the presence of ketones. These tests should always be performed during illness or stressful situations, when diabetes is likely to go out of control. The patient should also undergo yearly urine tests for microalbuminuria (small amounts of protein in the urine), a risk factor for future kidney disease.
Preventing Hypoglycemia
The following tips may help avoid hypoglycemia or prepare for attacks.
- Have a bedtime snacks if your blood glucose levels are below 180 mg/dL (10 mmol/L). Protein snacks may be best.
- Children (particularly thin children) may be at higher risk for hypoglycemia because the insulin injection goes into muscle tissue. Pinching the skin so that only fat (and not muscle) tissue is gathered or using shorter needles may help.
- Various insulin regimens are available that can reduce the risk. For example, taking a fast-acting insulin (insulin lispro) before the evening meal may be particularly helpful in preventing hypoglycemia at bedtime or during the night.
- Monitor blood glucose levels as often as possible, generally four times or more per day. This is particularly important for patients with hypoglycemia unawareness.
- Adults should be sure to monitor blood glucose levels before driving, when hypoglycemia can be very hazardous.
- Patients who are at risk for hypoglycemia should always carry hard candy, juice, sugar packets, or commercially available glucose substitutes.
- Patients at high risk for severe hypoglycemia, and their family members, should consider having on hand a glucagon emergency kit. The kit is available by prescription and contains an injection of glucagon, a hormone that helps to quickly raise blood glucose levels.
Family and friends should be aware of the symptoms and be prepared:
- If the patient is helpless (but not unconscious), family or friends should administer three to five pieces of hard candy, two to three packets of sugar, half a cup (four ounces) of fruit juice, or a commercially available glucose solution.
- If there is inadequate response within 15 minutes, the patient should receive additional sugar by mouth and may need emergency medical treatment, possibly including an intravenous glucose solution.
- Family members and friends can learn to inject glucagon (see above).
Patients with type 1 diabetes should always wear a medical alert ID bracelet or necklace that states that they have diabetes and take insulin.
Foot Care
Measures to Prevent Foot Ulcers. Preventive foot care can significantly reduce the risk of ulcers and amputation. Some tips for preventing problems include:
- Inspect your feet daily and watch for changes in color or texture, odor, and firm or hardened areas, which may indicate infection and potential ulcers.
- When washing the feet, the water should be warm (not hot) and the feet and areas between the toes should be thoroughly dried afterward. Check water temperature with the hand or a thermometer before stepping in.
- Apply moisturizers, but NOT between the toes.
- Gently use pumice to remove corns and calluses (do not use medicated pads or try to shave the corns or calluses by yourself).
- Trim toenails short and file the edges to avoid cutting adjacent toes.
- Well-fitting footwear is very important. Make sure your shoe is wide enough. Avoid high heels, sandals, thongs, and going barefoot. Shoes with a rocker sole reduce pressure under the heel and front of the foot and may be particularly helpful. Custom-molded boots increase the surface area over which foot pressure is distributed. This reduces stress on the ulcers and allows them to heal.
- Change shoes often during the day.
- Wear socks, particularly with extra padding (which can be specially purchased).
- Avoid tight stockings or any clothing that constricts the legs and feet.
- Consult a specialist in foot care for any problems.
Transplantation Procedures
Islet-Cell Transplantation
Researchers are investigating islet-cell transplantation as a way to help patients to come off insulin or reduce their use of it. Most research in recent years has focused on an islet-transplantation procedure called the Edmonton protocol.
This procedure has been used only in clinical trials, but it has helped some patients with severe type 1 diabetes to become free of insulin injections. However, many of these insulin-independent patients needed to resume insulin injections within 2 years. Researchers are continuing to work on refining the Edmonton protocol so that its benefits can be more sustainable and long lasting.
A major obstacle for the islet cell transplantation is the need for two or more donor pancreases to supply sufficient islet cells. Unfortunately, there are not enough pancreases available to make this procedure feasible for even 1% of patients. Researchers are looking for alternative approaches, including the use of umbilical cord cells, embryonic or adult stem cells, bone marrow transplantation, and other types of cellular therapies. These studies are still in very early stages, but researchers predict that there will be major advances in these fields in the coming years.
Organ Transplantation
Whole pancreas transplants and double transplants of pancreases and kidneys are proving to have good long-term success rates for some patients with type 1 diabetes. The operations help to prevent further kidney damage, and long-term studies indicate that they may even eventually reverse some existing damage. There is some evidence that heart disease and diabetic neuropathy improve after pancreas transplantation (although not retinopathy).
However, organ transplantation can have significant surgical and postsurgical complications. In addition, to prevent organ rejection, patients need to take immunosuppressive drugs on a lifelong basis following a transplant. Doctors generally recommend transplants in cases of end-stage kidney failure or when diabetes poses more of a threat to the patient's life than the transplant itself.
Resources
- www.diabetes.org -- American Diabetes Association
- www.niddk.nih.gov -- National Institute of Diabetes and Digestive and Kidney Diseases
- www.jdrf.org -- Juvenile Diabetes Research Foundation
- www.nei.nih.gov -- National Eye Institute
- www.eatright.org -- American Dietetic Association
- www.kidney.org -- National Kidney Foundation
- www.diabetestrialnet.org -- Type 1 Diabetes International Clinical Trial Net
- www.medicalert.org -- Bracelets or neck chain emblems with personal medical information
- www.childrenwithdiabetes.com -- Children with diabetes online community
References
Alemzadeh R and Wyatt DT. Diabetes mellitus. In: Kliegman RM, ed. Nelson Textbook of Pediatrics. 18th edition. Saunders; 2007:chap 590.
American Diabetes Association. Standards of medical care in diabetes -- 2012. Diabetes Care. 2012 Jan;35 Suppl 1:S11-63.
Bakris GL, Sowers JR; American Society of Hypertension Writing Group. ASH position paper: treatment of hypertension in patients with diabetes-an update. J Clin Hypertens (Greenwich). 2008 Sep;10(9):707-13; discussion 714-5.
Birkeland KI, Home PD, Wendisch U, Ratner RE, Johansen T, Endahl LA, et al. Insulin Degludec in Type 1 Diabetes: A randomized controlled trial of a new-generation ultra-long-acting insulin compared with insulin glargine. Diabetes Care. 2011 Mar;34(3):661-5. Epub 2011 Jan 26.
Camilleri M. Clinical practice. Diabetic gastroparesis. N Engl J Med. 2007 Feb 22;356(8):820-9.
Centers for Disease Control and Prevention (CDC). Use of hepatitis B vaccination for adults with diabetes mellitus: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2011 Dec 23;60(50):1709-11.
DCCT/EDIC Research Group, de Boer IH, Sun W, Cleary PA, Lachin JM, Molitch ME, et al. Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes. N Engl J Med. 2011 Dec 22;365(25):2366-76. Epub 2011 Nov 12.
de Kort H, de Koning EJ, Rabelink TJ, Bruijn JA, Bajema IM. Islet transplantation in type 1 diabetes. BMJ. 2011 Jan 21;342:d217. doi: 10.1136/bmj.d217.
Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group, Jacobson AM, Musen G, Ryan CM, Silvers N, Cleary P, et al. Long-term effect of diabetes and its treatment on cognitive function. N Engl J Med. 2007 May 3;356(18):1842-52.
Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group, Nathan DM, Zinman B, Cleary PA, Backlund JY, Genuth S, et al. Modern-day clinical course of type 1 diabetes mellitus after 30 years' duration: the diabetes control and complications trial/epidemiology of diabetes interventions and complications and Pittsburgh epidemiology of diabetes complications experience (1983-2005). Arch Intern Med. 2009 Jul 27;169(14):1307-16.
Farrar D, Tuffnell DJ, West J. Continuous subcutaneous insulin infusion versus multiple daily injections of insulin for pregnant women with diabetes. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD005542.
Fiorina P, Secchi A. Pancreatic islet cell transplant for treatment of diabetes. Endocrinol Metab Clin North Am. 2007 Dec;36(4):999-1013; ix.
Drueke TB, Locatelli F, Clyne N, Eckardt KU, Macdougall IC, Tsakiris D, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006 Nov 16;355(20):2071-84.
Hunt D. Foot ulcers and amputations in diabetes. Clin Evid. 2006 Jun;(15):576-84.
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group, Tamborlane WV, Beck RW, Bode BW, Buckingham B, Chase HP, et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med. 2008 Oct 2;359(14):1464-76. Epub 2008 Sep 8.
Pignone M, Alberts MJ, Colwell JA, Cushman M, Inzucchi SE, Mukherjee D, et al. Aspirin for primary prevention of cardiovascular events in people with diabetes: a position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation. Circulation. 2010 Jun 22;121(24):2694-701. Epub 2010 May 27.
Retnakaran R, Zinman B. Type 1 diabetes, hyperglycaemia, and the heart. Lancet. 2008 May 24;371(9626):1790-9.
SEARCH for Diabetes in Youth Study Group, Liese AD, D'Agostino RB, Hamman RF, Kilgo PD, Lawrence JM, et al. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006 Oct;118(4):1510-8.
Shapiro AM, Ricordi C, Hering BJ, Auchincloss H, Lindblad R, Robertson RP, et al. International trial of the Edmonton protocol for islet transplantation. N Engl J Med. 2006 Sep 28;355(13):1318-30.
Voltarelli JC, Couri CE, Stracieri AB, Oliveira MC, Moraes DA, Pieroni F, et al. Autologous nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus. JAMA. 2007 Apr 11;297(14):1568-76.
Writing Group for the SEARCH for Diabetes in Youth Study Group , Dabelea D, Bell RA, D'Agostino RB, Imperatore G, Johansen JM, et al. Incidence of diabetes in youth in the United States. JAMA. 2007 Jun 27;297(24):2716-24.
|
Review Date:
5/22/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |







